It’s hard to know where to even start with this update. The last few weeks have been unlike anything I’ve experienced in a very long time and pretty much everything I’ve been terrified of happening since March 2020. I do want to start by saying I am okay. I wouldn’t say I have fully recovered, but I am doing much better than I was and have complete confidence that I’ll make it to 100%, sooner rather than later, and without any long-term consequences. That said, four weeks ago, I got covid. And boy was it an experience. To be honest, and please pardon my language, but experience doesn't even do it justice. Absolute f*cking chaos is a much more accurate term.
Before I dive into the last few weeks, I feel like I need to take a moment to talk about how I got to where I am today and why I'm even writing this blog after such a long hiatus. For more than a decade, I shared my story and my life with chronic illness through a computer screen, with the hopes of both helping others, and finding much needed support through my struggles. Growing up with a chronic illness is hard. It’s isolating, for so many reasons. With CF, that isolation is amplified by the fact that we can’t have in-person support groups, because of the risk of sharing superbugs and making each other sicker. Instead, people in the cystic fibrosis community have turned to social media, eagerly and sometimes desperately seeking a connection with people who shared our burdens, seeking something that our “real life” family and friends simply couldn’t provide. Since high school, I’ve found solace and strength in being vulnerable with complete strangers. I’ve shared my fears and frustrations, my dreams and deepest desires. I took my passion for writing and used it connect with people all around the world, forging friendships that to this day, are some of the best I have. As a teenager, my reasons were more selfish than not. I’m a talker and my way of dealing with things is to just let it all out. Being able to vent to Facebook was a coping mechanism to try and manage all the stress that comes with this life and illness. I was in pain and angry. I was fatally ill and terrified. I needed to know it was going to be okay. I needed support and just encouragement through my daily fight against this disease.
As I got older though, I started to see the bigger picture. I started to see how deeply chronic illness affects people, how little the general public understands what it means to be chronically ill, and how broken our healthcare system is at times. I quickly realized how me being willing to talk about my experience could help others. I could help people feel like they weren’t alone while they were fighting their own battles — people who were feeling like I had just a few years earlier — and I could also help those who haven’t experienced adversity with their own health to understand a little better what their loved ones or peers who had might be feeling. By the time I was in college, I had a developed a passion for advocacy and doing everything I could to leave the chronic illness community better than it was when I first stepped into it.
Fast forward to 2020 and I found myself in a unique position.
 |
| A little visual comparison: The left was taken in 2019 when I weighed just 94lbs. The right was summer of 2021 at 115lb with no feeding tube. |
As amazing as this new reality was though, it did a number on my head. It’s been a paradigm shift of epic proportions. I’ve lived nearly 30 years preparing for a certain kind of future —one that wasn’t going to exist, to be blunt — and now all the sudden, I had infinitely more possibilities in front of me. It’s more than just having hope now. I have options, I have real tangible opportunities now. I’ve never been a fan of or made a “five year plan.” It seems so futile when there was a very real possibility I wouldn’t live another five years. Anyone who knows me know that I tend to live my life at a rate of 100mph. I throw myself into any and everything in an attempt to make the most of the time I have, knowing that time would run out earlier than I wanted. This was the only way I knew how to live and it worked for me… until Trikafta. Trikafta changed everything I thought I knew about what I wanted from my life. It forced me to really slow down and reflect. I had to try and work through things in my head and in my heart to decide what I wanted this new future to be. Which included trying to learn how to let go of the fear, doubt and anxiety that up until now, was ingrained in my very existence. I also turned 30 this year, which is huge and a milestone for anyone, CF or not. Generally speaking, most people see their 20s as the decade they go hard and “live life” as a single person. But in your 30s, you’re supposed to start a family, buy a house, advance your career, etc. Things I didn’t think would be possible for me before, but now actually had to consider. Couple all of that with the immense virtual fatigue we all felt because of covid, I realized that this online space wasn’t a safe space for me anymore. The openness and publicity of sharing my life online wasn't what I wanted or needed, so I let things go quiet.
So, what does that all have to do with now? Ha, that’s a great question. No surprise to anyone I’m sure, this turned into a novel of an update, so thank you to anyone who’s made it this far. In the last week or two, I found myself, for the first time in a while, wanting and needing that safe space again. I felt exhausted and defeated, knowing things will be okay eventually, but desperately needing that extra push from my people. I am also frustrated because so much of what I experienced in the last month should have never happened and0 I know the only way things will ever change is if people are willing to talk about what's going wrong.
In early November, I got Covid. It was, officially, the first time I got Covid in that it was my first positive test.
However, I also had covid in August. Yes, as in less-than-three-months-ago August. I never tested positive, but I had all the symptoms and had a very close and prolonged exposure (I spent two days on a tour bus for a work event and half a dozen participants tested positive by the following Monday). Both my UNC and Duke teams are in agreement that I had covid, just for whatever reasons wasn’t testing positive. I had a relatively mild case in August though. It wasn’t pleasant, felt like a bad flu virus but not horrible. Fast forward to early November and I travelled to visit family on the west coast. I started showing mild symptoms within a few days of traveling and did a home test. It was positive so I went to urgent care for confirmation. Sure enough, the rapid test at urgent was also positive. This time, since I did actually test positive, I was given Paxlovid, plus one week of high dose steroids and oral antibiotics to cover my chronic infections and hopefully avoid a CF exacerbation. I actually felt pretty good the first several days. The tiniest bit of congestion and that was it. No fevers, no crazy symptoms. I thought I had lucked out because I had recently gotten a booster, plus some natural immunity from August, and early intervention with Paxlovid, so I figured maybe I was going to be just fine and have a super mild case this time.
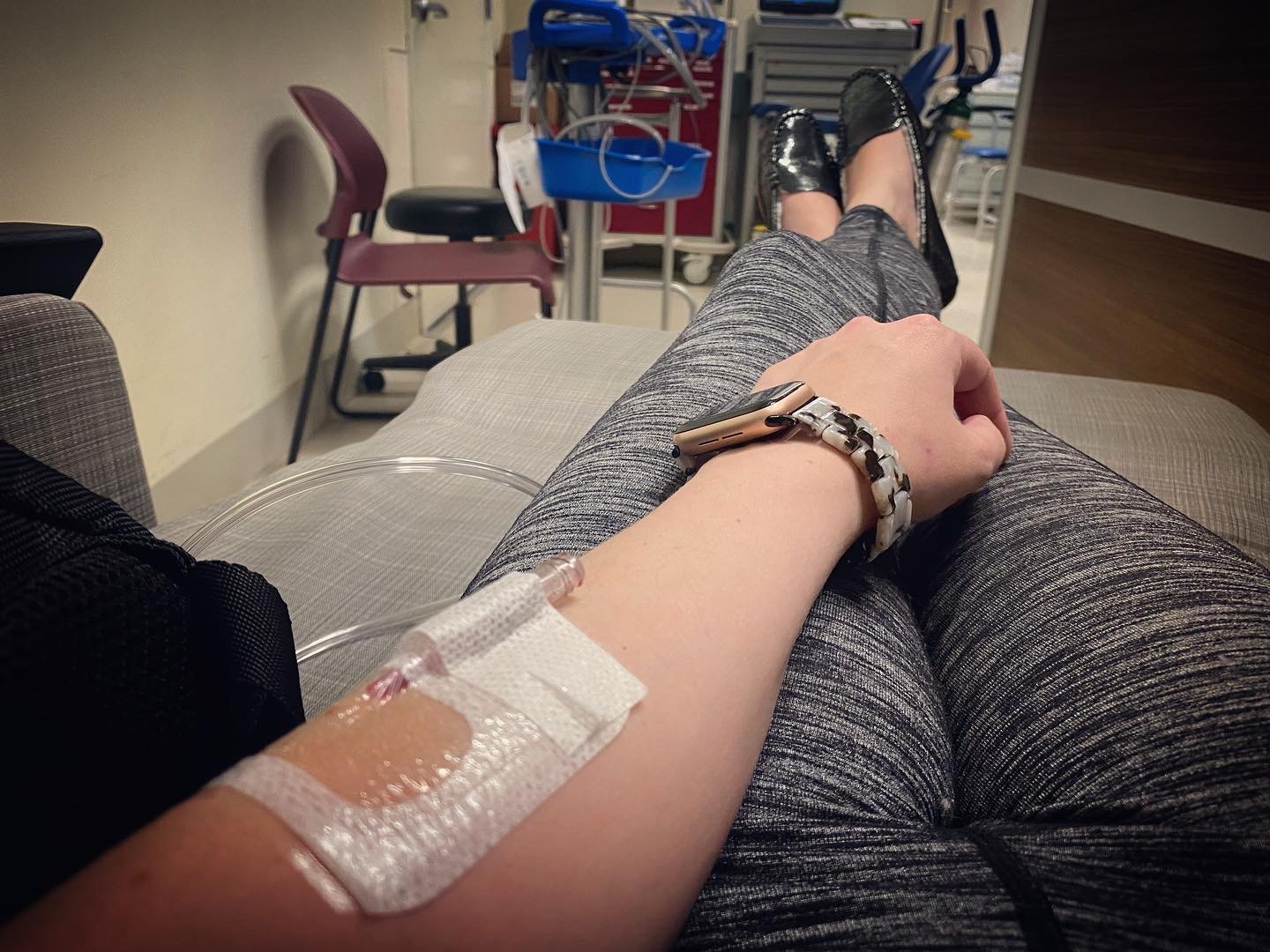
Around day 6, things started to go downhill. I started getting worse and by day 8, I was hypoxic and my O2 saturation was barely maintaining 90% at rest and dropping to 82-84% with even the mildest activity (walking for more than 3-4 mins, carrying more than 5lbs). My heartrate was also sitting at 130 at rest and spiking as high as 160+ with mild activity. I would have to sit with my portable oxygen concentrator for several minutes every time I had another tachycardic/hypoxic episode, waiting for it to pass. I called my team at UNC and we agreed that the best decision was for me to be inpatient for monitoring, additional testing and to get back on steroids and antibiotics while we figured this out. I didn’t feel comfortable traveling three hours alone to be admitted to UNC though, so the plan was to go to a local hospital and have my team coordinate with the doctors there to get a game plan in place. Ideally, a few days inpatient for a full work up (labs, xray, viral panel, etc) to make sure we weren’t missing something else — i.e. did I get RSV or flu on top of Covid, plus steroids and monitoring until my vitals were stable, then home on IV therapy for a full “tune up” since it’s been over 18 months since I did IVs. The working diagnosis was that I was having complications from Covid, but it had probably also stirred up a bit of a flare up of my usual CF bugs as that’s not uncommon when someone with CF gets a virus.
I went to the hospital on Tuesday night, (Nov. 15th) and after over 21 hours in the ER, I was admitted to an inpatient medicine ward the following evening.
 |
| How I feel about being on hourly glucose checks |
Emotionally and mentally though, this admission pushed me to a point of brokenness I have never felt before.
Overall, it was just a very poorly managed and very chaotic, very frustrating experience. For the time being, I don’t want to get into detail about things here online. It won't help and I want to maintain some discretion, as I will be pursuing more formal action with the hospital regarding some specific incidents that happened. But I can summarize by saying there was a huge lack of communication, transparency and trust, and there were a lot of errors made. A lot. Everything from the medical staff/physicians, to the nursing staff, to the general care and management of the hospital (food service, housekeeping, pharmacy, etc). Mistakes were made that honestly, had I not been able to advocate for myself and refuse or demand otherwise, damn well could have killed me. It was just one thing after another, after another to the point that I was genuinely considering discharging myself against medical advice.
Ultimately, I was able to work with the providers that I didn’t have to leave AMA — it's not exactly something you want on your medical record as a chronic illness patient. But I still wanted to go home as quickly as possible. The plan was never to stay inpatient since I have plenty of experience with home infusion therapy and the environment at the hospital was clearly not one that was benefiting me. After five days, my vitals were stable enough for me to go home. My tests all came back negative so there weren’t any additional complications or diagnoses, after the covid. I got home last Saturday (Nov 19) with the intention of finishing a full two course of IV antibiotics via home infusion therapy and my mediport. I have spent the last week and a half resting in the comfort of my house with the pups. Most of last week was spent sleeping and trying to recover, physically and emotionally.
 |
| Ready to go home! |
Emotionally, I am in a much better place today than last week, but still don’t feel like I’m completely myself yet.
This was a very traumatic experience and it’s going to take time to heal. This admission, juxtaposed against the fact that I’ve spent the last two years trying to reframe my perspective on life away from being the “sick girl” and figure out what my “new normal” looked like, was a lot to process. It was triggering and brought back so many emotions and feelings. It took me back to a time when I was much sicker. When I didn’t have hope and didn’t think I would ever get to experience many of life’s sweetest joys and milestones. When I spent every day worrying when it would all come crashing down. One of the biggest adjustments I’ve been working on as a part of my journey with Trikafta is letting go of the constant state of anxiety I lived in. Being able to move past the feeling that I was always just waiting for the evitable. Although I am okay now and nearly recovered from my bout with covid, it’s been really hard over the last two weeks to not let my mind go to that place again. I keep having to remind myself that this was an outlier. I got covid, and then had a very negative medical/hospital experience. It wasn’t my CF progressing. It wasn’t that Trikafta didn’t work anymore. If anything, the stability Trikafta has given me allowed me to survive what previously would have probably have killed me. This was a speed bump, not a complete detour, from the new direction my life is headed.
I don’t know if anyone will read this entire post, but that’s okay. I started writing it the day I got home but it’s taken me nearly two weeks to finish, and that’s okay too. I needed to get some of this out of my head and onto paper (well, onto a screen) and I needed to give myself time to process it. I’m choosing to share it publicly all now though for the same reason I shared earlier... because I know that I have a tribe of people who will support me as I continue to heal, and because I hope and believe that it can help someone else. I know I am not the only person with CF who is struggling to find their footing in a post-Trikafta world. This is new territory for us and it’s scary. I consider myself a pretty self-aware person and I’ve always been open about the mental health struggles that come with chronic illness. I’ve known that I needed to give myself grace as I figured out this new chapter of life, and I thought I was doing that. I thought I was doing okay. But the truth is it took getting covid and being throw headfirst back into a very broken healthcare system for me to realize just how not okay I actually am. It seems ridiculous to say that I am “not okay” about having a better quality of life and better prognosis than I use to. At times, I’ve felt guilty and questioned why I wasn’t just happy about it. But that’s the thing about trauma and grief. It’s not rational. It doesn’t make sense. And that’s okay. It doesn’t make me ungrateful. It doesn’t make me a bad person. It just makes me human. So if you’re reading this and you find yourself in the same place I did, feeling confused or overwhelmed by the changes and unsure where to go next, just know you’re not alone.
And for the rest of the world that reads this, thank you for listening. Thank you for always lifting me up and letting this virtual space be somewhere I could find comfort. Thank you to those of you who know me IRL and have supported and loved me for years. Thank you especially to the friends who knew what was going on this last month and went out of their way to help me with everything from bringing me food and watching my pups, to stepping in to covering my responsibilities at work or Junior League, and everything in between.
 |
| Happily back at home with my sweet boys |
As for what’s next, I’m not totally sure. I don’t know yet how active I’ll be on here moving forward, just that after a long hiatus, a part of me actually wanted to get on here and start sharing some of my life again. How much I post from here on is still TBD and it's definitely going to look different than it used to. My life is different now. We’ve come a long way in the cystic fibrosis community, and for that I am forever grateful, but one thing that became abundantly clear to me over the last month is that as a country, the healthcare industry is still catastrophically broken. We didn’t exactly have a stellar program going into the pandemic, but post-covid, the system is falling apart at the seams and failing on every level. We simply must do better. I don’t know how just yet, but I want to be a part of the solution.

No comments:
Post a Comment